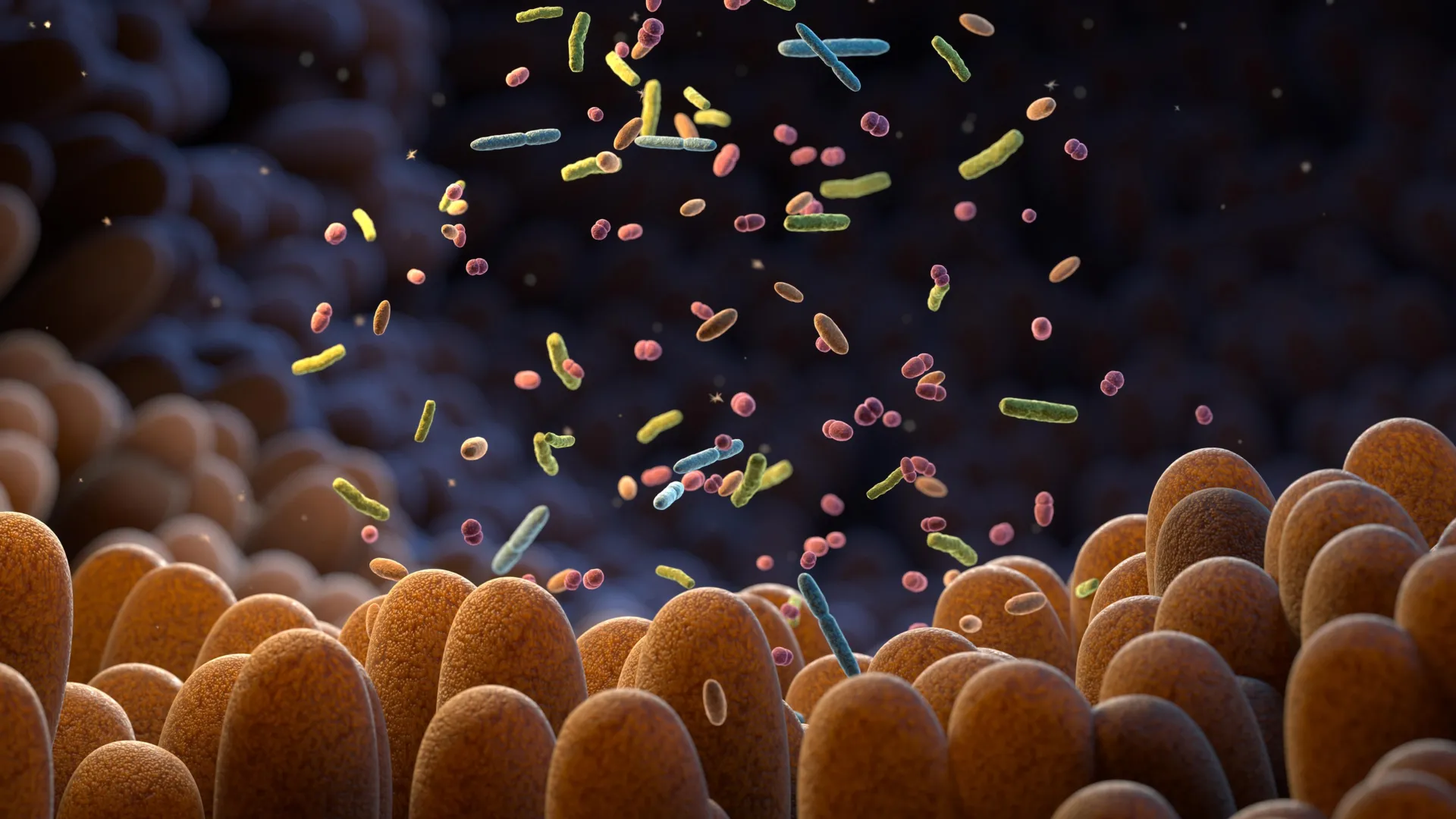
Chemotherapy is widely known to damage the lining of the intestines. While this effect is often treated as a localized problem, the consequences extend beyond the digestive tract. When the intestinal lining is injured, the availability of nutrients inside the gut changes, forcing resident bacteria to adapt to a new environment.
Researchers found that damage to the intestinal lining caused by chemotherapy alters how gut bacteria access nutrients. As a result, the makeup and behavior of the microbiota shift. One key change is an increase in the production of indole-3-propionic acid (IPA), a microbial compound derived from the amino acid tryptophan.
A Microbial Signal With Bodywide Effects
IPA does not remain confined to the gut. Instead, it acts as a signal that travels through the body to the bone marrow, where immune cells are produced. Higher levels of IPA change this process, altering myelopoiesis and lowering the production of immunosuppressive monocytes. These monocytes normally help cancer cells evade immune defenses and support the growth of metastases.
“We were surprised by how a side effect often seen as collateral damage of chemotherapy can trigger such a structured systemic response. By reshaping the gut microbiota, chemotherapy sets off a cascade of events that rewires immunity and makes the body less permissive to metastasis,” says Ludivine Bersier, first author of the study.
This shift in immune cell production boosts T cell activity and changes how immune cells interact within areas where cancer spreads. The effect is especially clear in the liver. In preclinical models, these changes create conditions that are resistant to metastatic growth.
Evidence From Cancer Patients
The findings from laboratory studies are supported by patient data. Clinical relevance was confirmed using data collected in collaboration with Dr. Thibaud Koessler (Geneva University Hospitals, HUG). Among patients with colorectal cancer, those with higher levels of IPA in the bloodstream after chemotherapy showed lower monocyte levels. This immune profile is associated with better survival outcomes.
“This work shows that the effects of chemotherapy extend far beyond the tumor itself. By uncovering a functional axis linking the gut, the bone marrow, and metastatic sites, we highlight systemic mechanisms that could be harnessed to durably limit metastatic progression,” says Tatiana Petrova, corresponding author of the study.
Long Term Immune Effects and Future Potential
The research received support from several organizations, including the Swiss National Science Foundation and the Swiss Cancer League. An ISREC Foundation Tandem Grant enabled close collaboration between clinical and basic research, led at Unil by Professor Tatiana Petrova and Dr. Thibaud Koessler at HUG. The team proposes that chemotherapy may create a form of biological “memory,” driven by metabolites produced by gut microbes that continue to suppress metastatic growth over time.
Taken together, the results point to a previously underappreciated gut-bone marrow-liver metastasis axis. This pathway helps explain how chemotherapy can produce lasting effects throughout the body and suggests new ways to use microbiota-derived metabolites as supportive strategies to limit the spread of cancer.